Integrating GenAI and Precision Medicine in Brain Tumor Research: Implications for Advanced Biomedical Education and Clinical Practice

Brain tumors present a unique set of challenges in both diagnosis and treatment, given the vast heterogeneity in tumor types, locations, and individual patient responses. The complexity of brain tumors requires a multidisciplinary approach to treatment that can integrate the latest advancements in medicine and technology. One such breakthrough is the integration of precision medicine and generative artificial intelligence (GenAI), two transformative technologies that have the potential to revolutionize both the research and clinical management of brain tumors.
Precision medicine aims to provide personalized treatment plans based on an individual’s genetic, environmental, and lifestyle factors, offering a more targeted and effective approach compared to traditional one-size-fits-all treatments. When combined with GenAI, which excels at analyzing large datasets and generating predictive models, the potential to enhance brain tumor research and clinical practice becomes profound. This article explores how the integration of GenAI and precision medicine in brain tumor research is shaping the future of biomedical education and clinical practice.
Understanding Precision Medicine in Brain Tumor Research
Precision medicine is an approach that tailors treatment strategies to the unique genetic makeup of each patient. In the context of brain tumor research, this method utilizes genomic profiling, where sequencing technologies such as next-generation sequencing (NGS) are used to map the genetic changes within tumor cells. These genomic profiles help clinicians better understand the underlying mechanisms driving tumor growth and metastasis, ultimately guiding decisions about the most appropriate treatment options.
Targeted therapies are a key component of precision medicine, designed to target specific genetic mutations or protein expressions that drive the tumor’s growth. Unlike traditional therapies, which treat the tumor broadly, targeted therapies aim to disrupt these processes with minimal impact on surrounding healthy tissue. This approach has shown promising results in several tumor types, and as the field of brain tumor research continues to advance, the hope is to significantly improve patient outcomes.
However, implementing precision medicine in clinical practice comes with its own set of challenges. The complexity and volume of data generated by genomic and clinical profiling can be overwhelming for clinicians without the right tools to interpret it. Moreover, precision medicine requires a multidisciplinary approach, involving geneticists, oncologists, radiologists, and other healthcare providers, to ensure a comprehensive treatment strategy for each patient.
Generative AI and Its Role in Brain Tumor Research
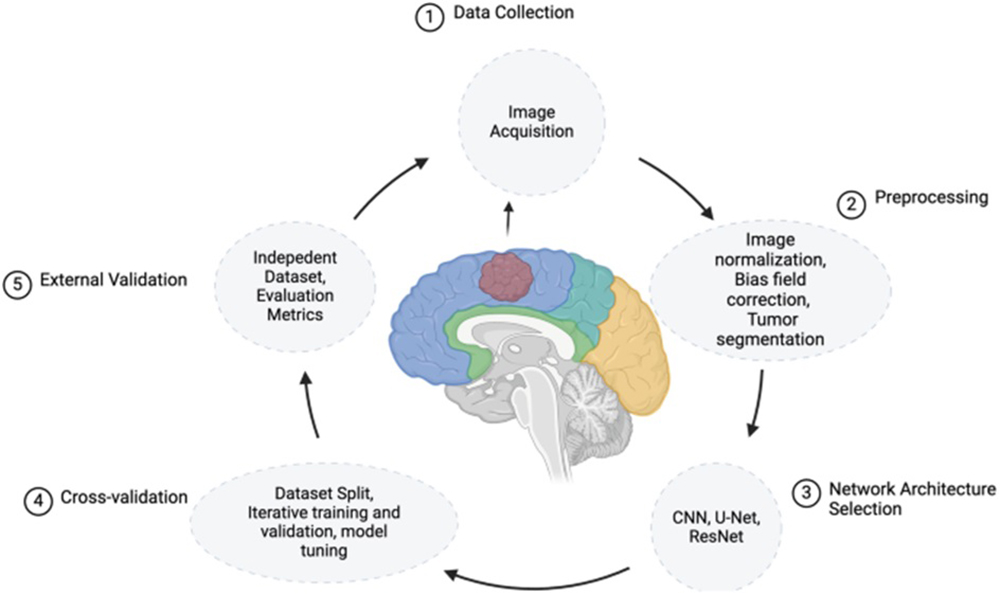
Generative AI is increasingly being recognized for its potential in biomedical research, particularly in oncology. By leveraging advanced machine learning algorithms, GenAI can analyze vast amounts of data from multiple sources, including genetic sequences, clinical records, and medical imaging, to generate predictive models that can inform decision-making. These models can predict tumor behavior, patient responses to treatment, and long-term outcomes, offering clinicians powerful tools to personalize treatment plans.
One of the most promising applications of GenAI in brain tumor research is in drug discovery. AI models can simulate the interactions between drug compounds and molecular targets within tumor cells, helping to identify promising drug candidates. This is particularly valuable in the context of brain tumors, where the blood-brain barrier often limits the effectiveness of many traditional drugs. GenAI can also be used to identify novel biomarkers, which are essential for early detection, prognosis, and monitoring the effectiveness of therapies.
Moreover, GenAI has the potential to improve diagnostic accuracy. For example, AI-driven image processing algorithms can analyze MRI and CT scans to identify subtle changes in tumor size or structure that might be missed by human eyes. By enhancing the precision of tumor detection and tracking, GenAI enables clinicians to make more informed decisions about treatment plans.
Implications for Advanced Biomedical Education
As GenAI and precision medicine continue to transform brain tumor research, their integration into biomedical education is paramount. To fully realize the potential of these technologies, future biomedical professionals need to be equipped with the knowledge and skills to work with genomic data, AI tools, and personalized treatment strategies.
Educational programs should incorporate courses that focus on the intersection of AI, genomics, and clinical practice. For example, students could learn how to use bioinformatics tools to analyze genetic data, apply AI algorithms to predict treatment outcomes, and collaborate in interdisciplinary teams to design personalized treatment plans. Additionally, the development of specialized AI-driven simulations and case studies could help students understand the complexities of diagnosing and treating brain tumors, providing a more interactive and practical learning experience.
Interdisciplinary collaboration is another crucial aspect of advanced biomedical education. The integration of AI and precision medicine requires expertise from multiple fields, including data science, bioinformatics, oncology, and clinical practice. Educational institutions should foster environments where students from these diverse disciplines can work together to solve complex healthcare challenges, preparing them to apply their knowledge in real-world settings.
Clinical Practice and Implementation
In clinical practice, the integration of GenAI and precision medicine has the potential to revolutionize how brain tumors are diagnosed, treated, and monitored. GenAI can assist clinicians in making more accurate and data-driven decisions by analyzing complex datasets and generating personalized treatment recommendations. For instance, AI-driven clinical decision support systems (CDSS) can help clinicians select the most appropriate therapies based on a patient’s genetic profile and tumor characteristics.
One of the key benefits of these technologies is the ability to provide more personalized treatment plans. Traditional treatment approaches often rely on generalized protocols that may not account for the unique characteristics of each patient’s tumor. By incorporating genomic data and AI-powered predictions, clinicians can tailor treatment strategies to maximize efficacy and minimize side effects. This approach has the potential to improve patient outcomes, particularly in difficult-to-treat brain tumors.
However, the implementation of GenAI and precision medicine in clinical practice also presents challenges. These include ensuring data privacy, obtaining patient consent for genetic testing, and navigating the ethical implications of AI-based decision-making. There is also the need for continuous validation of AI models to ensure their accuracy and reliability in clinical settings.
Future Directions
Looking ahead, the future of brain tumor research and treatment lies in continued innovation and collaboration. AI-driven advances in tumor biopsy and imaging are expected to improve early detection and monitoring of brain tumors. Non-invasive diagnostics, such as liquid biopsies, combined with AI analysis, could provide clinicians with real-time insights into tumor progression and treatment response.
Furthermore, collaborative research networks that bring together experts from diverse fields will be essential in advancing both GenAI and precision medicine. These networks will help accelerate the development of new treatments, identify promising biomarkers, and ensure that innovative therapies are accessible to all patients, regardless of their geographic location.
The integration of GenAI and precision medicine in brain tumor research is poised to transform both the way we understand these complex diseases and how we treat them. By personalizing treatment strategies based on genetic data and harnessing the power of AI to predict tumor behavior, clinicians can make more informed decisions that improve patient outcomes. For biomedical education, this shift requires the integration of AI, genomics, and interdisciplinary collaboration into curricula, ensuring that future professionals are prepared to navigate the complexities of this rapidly evolving field. As we look to the future, the continued convergence of GenAI, precision medicine, and clinical practice offers the promise of more effective, personalized care for brain tumor patients, ushering in a new era of medical breakthroughs.
Related News
Apply Now: French Embassy Research Scholarships 2025 Open for Applications
The French Embassy in Sri Lanka and the Maldives is proud to announce the opening of its annual call for applications to…
Read MoreGCE A/L Results Release Update – www.doenets.lk
The Department of Examinations has announced that the results of the 2024 G.C.E. Advanced Level examination will be released after April 20.…
Read MoreAngelo Mathews Named Brand Ambassador for The Next Education Consultancy & BIMT Campus
In a landmark move that bridges excellence in education with the spirit of sporting greatness, The Next Education Consultancy and BIMT Campus…
Read MoreAustralasian Academy Hosts Thrilling Inter-Culinary Competition 2025
The culinary scene at Australasian Academy was set ablaze with talent and passion as students showcased their exceptional culinary skills at the…
Read MoreEmbassy of Sri Lanka in Washington, D.C. facilitates partnership between NSBM Green University and American University
The NSBM Green University Sri Lanka and the American University (AU) Washington, D.C. formalized an academic partnership, marking a significant milestone in…
Read MoreCourses
-

IMC – Bachelor of Psychology
IMC Education Overview IMC Campus in partnership with Lincoln University College (LUC) Malaysia offers Bachelor of Psychology Degree right here in Sri… -
ANC – BA (Hons) International Business Management (Top-Up)
ANC Education Overview Designed in partnership with public and private business organizations, this program develops one’s ability to critically evaluate business models… -
IIT – BSc (Hons) Computer Science
IIT Campus Overview BSc (Hons) Computer Science provides a solid foundation and training regarding the fundamentals of the computer science field, along… -

APIIT – BSc (Hons) Cyber Security
APIIT Sri Lanka Overview Our BSc (Hons) Cyber Security award is designed to launch your future career in the protection of software… -

ICBS – BSC (Hons) Business Management with Marketing Management
ICBS Overview The BSc (Hons) Business Management with Marketing program, awarded by Queen Margaret University (QMU), is a highly regarded degree that… -

UTS – Diploma of Science
UTS College Sri Lanka Overview The Diploma of Science is designed to empower you to apply scientific thinking and analysis to important… -

CSA – Master of Architecture and Environmental Design
City School of Architecture Overview The Master of Architecture and Environmental Design Degree at CSA is awarded by the University of the… -

APIIT – BSc (Hons) International Business Management
APIIT Sri Lanka Overview Increasingly businesses are becoming more and more international. This requires business management professionals to have knowledge, skills and… -
IIT – BSc (Hons) Artificial Intelligence And Data Science
IIT Campus Overview The BSc (Hons) Artificial Intelligence and Data Science course is awarded by Robert Gordon University (RGU) in the UK… -

ICBS – International Degree Foundation in Business / IT
ICBS Overview The Scottish Qualification Authority (SQA) is a globally recognized organization dedicated to education and qualification development. SQA is responsible for… -

APIIT – BA (Hons) Finance and Business Enterprise
APIIT Sri Lanka Overview Finance and accounting are no longer just about taxation and the management of financial capital. This award will… -

APIIT – MBA General
APIIT Sri Lanka Overview The MBA is awarded by Staffordshire University, UK. This award is an advanced course of study in management… -
ANC – LLM in International Business & Commercial Law
ANC Education Overview This course is designed for graduates of law, business and finance in a legal or a corporate job role… -

AOD – BA (Hons) Fashion Design and Marketing
Academy of Design Overview The syllabus is from the UK’s Northumbria University, as one of their most revered flagship programmes and is… -

APIIT – MSc. Marketing Management
APIIT Sri Lanka Overview This MSc Marketing Management degree – awarded by Staffordshire University, UK is an advanced course of study in…
Newswire
-

Underworld gang arrested with weapons
ON: April 19, 2025 -

IPL points table 2025 | Standings
ON: April 19, 2025 -

Sri Lanka thrash Malaysia to keep Rugby World Cup hopes alive
ON: April 19, 2025 -
5.8 magnitude earthquake jolts Afghanistan, tremors felt in India, Pakistan
ON: April 19, 2025